Perioperative Medication Safety: Why Surgical Teams Need Better Decision Support
15 October, 2025
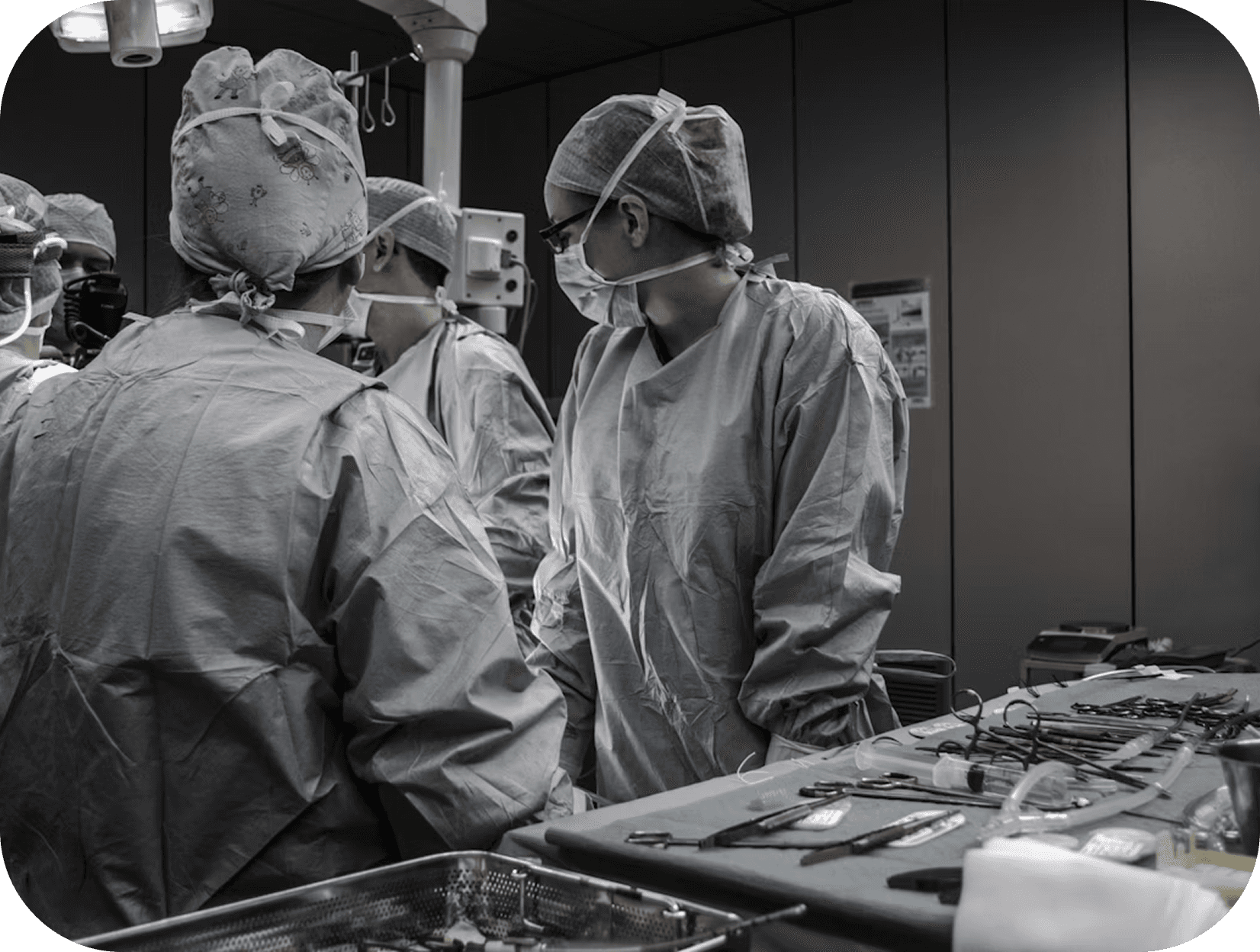
The perioperative period represents one of the highest-risk phases of patient care, where medication errors can have immediate and severe consequences. Surgical teams face unique prescribing challenges that demand smarter, faster decision-making tools.
Surgery involves rapid clinical decisions, often under time pressure and in complex, evolving situations. Anaesthetists, surgeons, and ward teams must coordinate medication plans across multiple phases of care. Pre-operative assessments require careful review of existing medications, many of which need to be withheld or adjusted. Intraoperative drug administration demands precise dosing and consideration of drug interactions under anaesthesia. Post-operative management involves pain control, antibiotic prophylaxis, thromboprophylaxis, and resumption of chronic medications.
Each transition creates potential for error. Medications may be continued when they should be stopped, or stopped when they should be continued. Drug interactions with anaesthetic agents can be overlooked. Dosing adjustments for renal or hepatic impairment may be missed in the urgency of surgical care.
Common Perioperative Medication Challenges
Anticoagulation Management: Balancing bleeding risk against thrombotic risk requires careful timing of medication cessation and restart. Guidelines vary by procedure and patient factors, creating complexity that can lead to errors.
Chronic Medication Continuation: Deciding which medications to continue through surgery requires understanding of both pharmacology and surgical risk. Beta-blockers, antihypertensives, and medications for chronic conditions need individualised plans.
Drug Interactions with Anaesthesia: Certain medications interact dangerously with anaesthetic agents, requiring identification and management before surgery begins.
Post-operative Prescribing Gaps: After surgery, patients may not receive their usual medications promptly, or may receive inappropriate combinations during the recovery phase.
The Role of AI in Surgical Medication Safety
AI-powered clinical decision support can address these challenges by providing real-time, context-aware guidance. When a surgical patient is admitted, AI systems can instantly analyse their medication history, flag potential concerns, and suggest evidence-based management strategies.
For pre-operative assessment, AI can identify medications requiring cessation or continuation, provide timing recommendations, and alert teams to potential anaesthetic interactions. During post-operative care, it can ensure appropriate resumption of chronic medications and flag new prescriptions that may interact with existing therapies or surgical considerations.
The value lies not in replacing clinical judgment, but in preventing oversights in high-pressure environments. Surgical teams benefit from having comprehensive medication safety checks integrated seamlessly into their workflow, reducing cognitive load and improving consistency of care.
As surgical volumes increase and patient complexity grows, technology that supports safer perioperative medication management becomes essential. The goal is straightforward: ensure every surgical patient receives the right medications at the right time, with full consideration of their individual clinical context.
Better decision support means better outcomes, fewer complications, and more efficient surgical care for everyone.
More blogs

Half of All Drug Interaction Events Are Preventable. So Why Aren't We Preventing Them?
Adverse drug interactions are responsible for thousands of hospital admissions each year, and half of them are entirely preventable.

The Future of AI in Healthcare: One Super AI or Many Smart Tools?
As artificial intelligence evolves, clinicians and healthcare leaders face a critical question: Will one all-powerful AI dominate, or will we rely on a constellation of smaller, specialised systems working together in harmony?

America's Prescription Problem: When the Cure Becomes the Third Most Deadly Threat
A sobering reality has emerged in American healthcare: adverse drug events (ADEs) have now become the third leading cause of death in the United States, according to recent analysis by the American Society of Pharmacovigilance.